Arthritis is a term that encompasses a diverse group of inflammatory joint disorders that affect millions of people worldwide. As a leading cause of disability, arthritis can profoundly impact an individual’s quality of life, making everyday activities challenging and painful. The condition is characterized by joint pain, stiffness, swelling, and a decreased range of motion, which can vary in severity and impact daily functioning.
Understanding arthritis involves not only recognizing its various forms but also grasping the underlying causes and symptoms that differentiate them. Osteoarthritis, the most common type, is primarily a degenerative joint disease that results from the gradual wear and tear of cartilage. Rheumatoid arthritis, on the other hand, is an autoimmune disorder where the body’s immune system mistakenly attacks the joints. This distinction is crucial for tailoring effective management strategies.
Managing arthritis effectively requires a multifaceted approach that integrates medical treatments, lifestyle modifications, and complementary therapies. From conventional medications that reduce inflammation to physical therapy that maintains joint function, there are numerous ways to address the symptoms and enhance well-being. This article explores the different facets of arthritis, including its causes, symptoms, and a comprehensive overview of management strategies, to provide a holistic understanding of how to cope with and manage this chronic condition.

(commons.wikipedia)
Symptoms of Arthritis
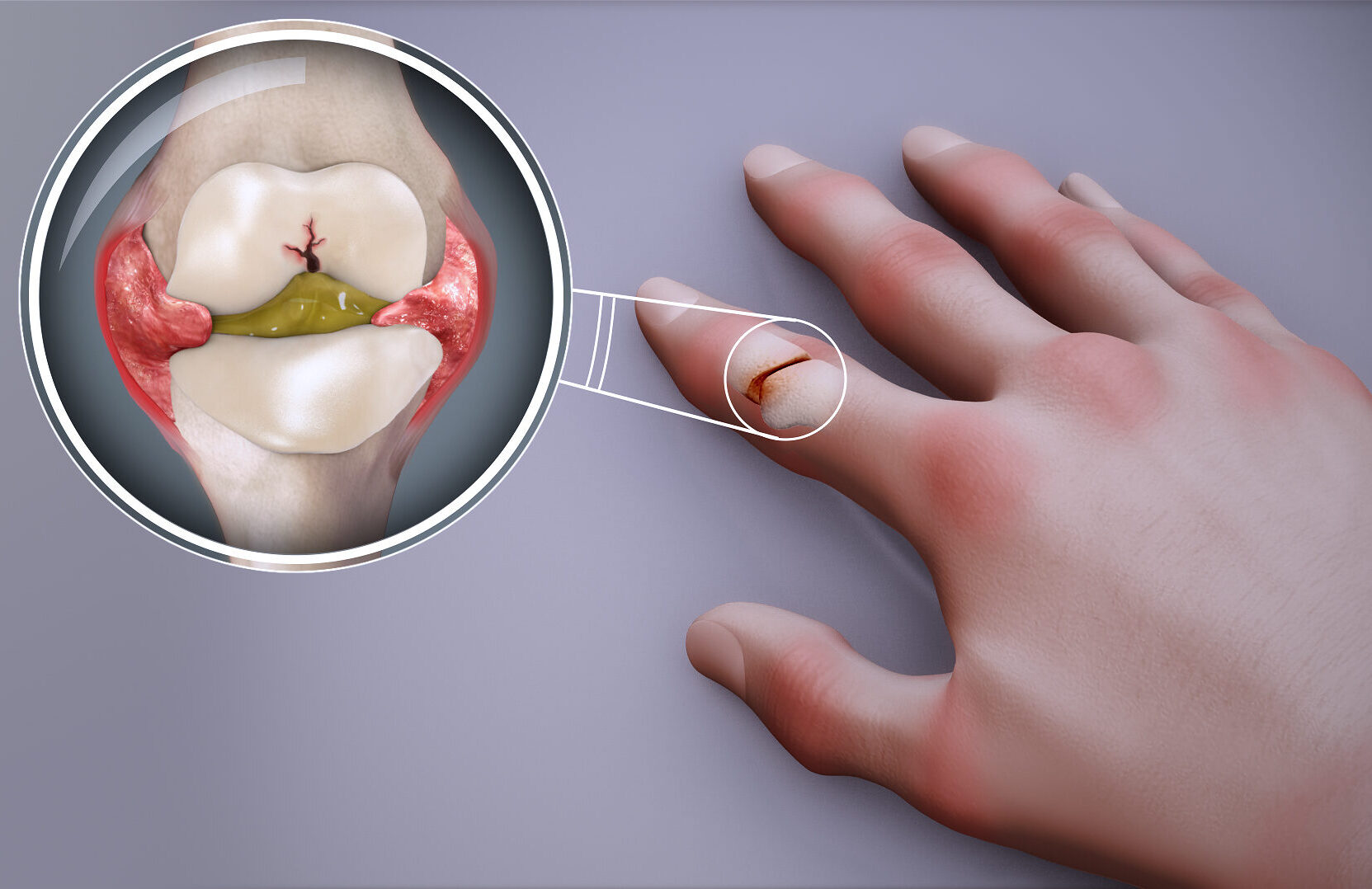
Arthritis primarily manifests as joint pain, swelling, stiffness, and a decreased range of motion, significantly impacting daily activities and overall quality of life. These symptoms can vary in intensity, from mild discomfort to severe pain, and can be constant or intermittent. The affected joints may feel warm to the touch, appear red, and can become deformed over time if the condition is not managed properly. Fatigue and general feelings of malaise are also common, especially in inflammatory types of arthritis such as rheumatoid arthritis. This chronic pain can lead to sleep disturbances and increased levels of stress and anxiety, further complicating the lives of those affected. Additionally, some forms of arthritis can cause a reduction in muscle strength and endurance due to decreased physical activity, exacerbating the impact on mobility and daily functioning.
The symptoms of arthritis are not limited to the physical; they can also have a profound impact on mental health. Persistent pain and decreased mobility can lead to feelings of frustration, helplessness, and depression. Many individuals with arthritis may find it challenging to participate in activities they once enjoyed, leading to social isolation. Additionally, the unpredictable nature of arthritis symptoms can make it difficult to plan daily activities, contributing to a sense of instability and insecurity. It’s crucial to address both the physical and psychological aspects of arthritis to improve overall quality of life for those affected. Understanding the full spectrum of arthritis symptoms can help individuals and healthcare providers develop comprehensive management plans that address all aspects of the disease.
(Osteoarthritis Symptoms)
Osteoarthritis (OA), the most common form, is primarily a degenerative joint disease where the cartilage that cushions the ends of bones wears down over time. This wear and tear can lead to bones rubbing directly against each other, causing pain, swelling, and reduced flexibility in the joint. The symptoms of OA often develop slowly and worsen over time. Commonly affected joints include the knees, hips, hands, and spine. Individuals with OA may experience a grating sensation or hear popping and cracking sounds when using the affected joint. As the disease progresses, bone spurs—extra bits of bone that feel like hard lumps—can form around the affected joint, further limiting movement and increasing discomfort. In severe cases, the joint may become unstable or even give way, leading to falls and additional injuries.
In advanced stages of OA, the pain can become debilitating, severely limiting mobility and independence. Everyday tasks such as walking, climbing stairs, or even gripping objects can become extremely painful and challenging. This loss of function can lead to a decrease in physical activity, which can have additional negative effects on overall health, including weight gain, muscle weakness, and decreased cardiovascular fitness. Managing OA often requires a combination of medical treatments, physical therapy, and lifestyle changes to slow the progression of the disease and maintain as much joint function as possible. Surgical interventions, such as joint replacement, may be considered when conservative treatments fail to provide adequate relief and improve quality of life.
(Rheumatoid Arthritis Symptoms)
Rheumatoid arthritis (RA) is an autoimmune disorder in which the body’s immune system attacks its own tissues, particularly the synovium—a soft tissue in the joints that produces fluid to lubricate them. This leads to inflammation, which can cause painful swelling and eventually result in bone erosion and joint deformity. RA often affects joints symmetrically, meaning if one knee or hand is affected, the other one usually is too. In addition to joint symptoms, RA can affect other parts of the body, including the skin, eyes, lungs, heart, and blood vessels, leading to a range of systemic symptoms such as fever, weight loss, and fatigue. The presence of these extra-articular manifestations underscores the systemic nature of RA and the need for comprehensive medical management.
The systemic nature of RA means it can cause widespread health issues beyond joint pain. Chronic inflammation associated with RA can lead to complications such as cardiovascular disease, lung disease, and osteoporosis. The constant pain and fatigue can also contribute to mental health issues, including depression and anxiety. Because RA can cause periods of increased disease activity, known as flares, managing the condition often requires ongoing medical treatment and lifestyle adjustments. Early diagnosis and treatment are crucial to prevent severe joint damage and systemic complications, helping individuals maintain a better quality of life. Advances in treatment, particularly the use of biologics and disease-modifying antirheumatic drugs (DMARDs), have significantly improved the prognosis for many people with RA.
(Other Forms of Arthritis)
Other types of arthritis, such as psoriatic arthritis, gout, and lupus, present with unique symptoms that distinguish them from OA and RA. Psoriatic arthritis, for example, can cause joint pain along with patches of red, scaly skin associated with psoriasis. This form of arthritis often affects the fingers and toes, leading to characteristic swelling known as dactylitis, or “sausage digits.” Gout typically affects the big toe but can occur in other joints, characterized by sudden, severe attacks of pain, swelling, redness, and tenderness. These attacks are caused by the accumulation of urate crystals within the joint, resulting from high levels of uric acid in the blood. Lupus, a systemic autoimmune disease, can cause arthritis along with a variety of symptoms affecting the skin, kidneys, brain, and other organs. Each type requires a tailored approach to treatment based on the specific symptoms and underlying causes.
The diversity in arthritis types and symptoms necessitates a comprehensive and individualized approach to diagnosis and management. For instance, gout management often involves dietary changes to reduce uric acid levels, while lupus treatment may focus on controlling immune system activity. Psoriatic arthritis might require both dermatological and rheumatological interventions. Understanding the specific type of arthritis is crucial for effective treatment, as it allows healthcare providers to develop targeted strategies to alleviate symptoms, prevent progression, and improve patients’ quality of life. Regular monitoring and adjustments to treatment plans are essential to address the evolving nature of these conditions and to ensure optimal management.
(Impact on Daily Life)
The symptoms of arthritis can severely impact daily life, making simple tasks challenging. Joint pain and stiffness can limit mobility and dexterity, affecting the ability to walk, climb stairs, grip objects, or perform routine activities such as dressing and cooking. The chronic nature of the pain and discomfort can lead to sleep disturbances, further exacerbating fatigue and impacting overall mental health. Individuals with arthritis often have to make significant adjustments to their daily routines to manage their symptoms and maintain their independence. This can include modifying work environments, utilizing assistive devices, and seeking help with household chores.
In addition to physical limitations, arthritis can also lead to emotional and social challenges. The constant pain and decreased ability to perform everyday activities can lead to feelings of frustration and depression. Social interactions may be reduced as individuals avoid activities that exacerbate their symptoms, leading to isolation. The financial burden of ongoing medical care, treatments, and potential loss of income due to decreased work capacity can add to the stress. Managing arthritis effectively requires a holistic approach that addresses both the physical and psychological aspects of the disease, including regular medical care, physical therapy, mental health support, and lifestyle modifications to improve overall well-being. Support from family, friends, and arthritis support groups can also play a crucial role in coping with the condition and maintaining a positive outlook.
Causes of Arthritis
The causes of arthritis are multifaceted, often involving a combination of genetic predisposition, lifestyle factors, and environmental triggers. Osteoarthritis (OA), the most common form of arthritis, is generally associated with aging, as the wear and tear on joints accumulate over time. Joint injury can accelerate the degeneration of cartilage, leading to early onset of OA. Obesity is a significant risk factor as it puts additional stress on weight-bearing joints like the knees and hips, exacerbating the deterioration of cartilage. Repetitive stress from occupations or activities that involve heavy lifting or prolonged standing can also contribute to the development of OA. Additionally, joint malformations or genetic conditions affecting cartilage can predispose individuals to OA.
Rheumatoid arthritis (RA) has a more complex etiology, involving genetic markers and immune system dysfunctions. Certain genetic markers, such as the HLA-DR4 allele, have been linked to an increased risk of developing RA. The exact cause of the immune system’s attack on joint tissues in RA is not fully understood, but it is believed to be triggered by a combination of genetic susceptibility and environmental factors. Infections, smoking, and exposure to certain viruses or bacteria have been suggested as potential triggers for the autoimmune response in RA. Hormonal changes, particularly in women, may also play a role in the onset of RA, as the disease is more prevalent in females and often begins during or after pregnancy or menopause.
(Environmental and Lifestyle Factors)
Environmental factors and lifestyle choices can significantly impact the risk and progression of arthritis. For instance, smoking is a well-known risk factor for RA, and cessation can improve treatment outcomes. Diet also plays a role; a diet high in processed foods and sugars can increase inflammation, while a diet rich in fruits, vegetables, omega-3 fatty acids, and whole grains can help reduce inflammation and support joint health. Regular physical activity is essential in managing arthritis symptoms and preventing progression, as it helps maintain joint flexibility and strengthens the muscles around the joints. However, overuse or improper exercise techniques can lead to joint injuries, which may contribute to OA.
Exposure to certain environmental factors, such as air pollution and occupational hazards, can also contribute to the development and exacerbation of arthritis. Workers in jobs that require repetitive motion, heavy lifting, or prolonged standing are at higher risk for developing OA. Additionally, a sedentary lifestyle can lead to obesity and poor joint health, increasing the likelihood of arthritis. Understanding the impact of these environmental and lifestyle factors can help individuals make informed choices to reduce their risk of developing arthritis or manage existing symptoms more effectively.
(Genetic Factors)
Genetics play a crucial role in the development of various forms of arthritis. Family history is a significant risk factor; individuals with close relatives who have arthritis are more likely to develop the condition themselves. Specific genetic markers have been identified that increase susceptibility to arthritis. For example, the presence of certain genes, such as those coding for the HLA class II antigens, has been associated with a higher risk of RA. Genetic factors also influence the severity and progression of the disease. In OA, genetic variations can affect cartilage metabolism, leading to early degradation and increased susceptibility to joint damage.
Research into the genetic basis of arthritis is ongoing, with the aim of identifying new genetic markers and understanding how they interact with environmental factors to cause the disease. This knowledge can potentially lead to the development of personalized treatments based on an individual’s genetic profile. For instance, individuals with a genetic predisposition to RA might benefit from early interventions and more aggressive treatment strategies to prevent severe joint damage. Genetic counseling may also be beneficial for those with a family history of arthritis, helping them understand their risk and take preventive measures.
(Infections and Immune System Dysfunction)
Infections can play a significant role in triggering certain types of arthritis. Reactive arthritis, for example, can occur after infections of the urinary tract, gastrointestinal system, or other parts of the body. These infections can trigger an immune response that mistakenly targets the joints, leading to inflammation and pain. In RA, it is believed that an infection or other environmental factor triggers the immune system to attack the synovium, leading to chronic inflammation and joint damage. The exact mechanisms by which infections trigger these autoimmune responses are not fully understood, but it is clear that the immune system plays a crucial role in the development of many types of arthritis.
Immune system dysfunction is a central feature in autoimmune forms of arthritis like RA and lupus. In these conditions, the immune system mistakenly attacks the body’s own tissues, causing inflammation and damage to the joints and other organs. Understanding the underlying mechanisms of immune system dysfunction can help in developing targeted therapies to modulate the immune response and reduce inflammation. Advances in immunology have led to the development of biologic drugs that specifically target components of the immune system involved in the inflammatory process, offering new hope for individuals with autoimmune arthritis.
Medical Treatments
Effective management of arthritis involves a holistic approach that combines medical treatment, lifestyle modifications, and supportive therapies. Medications, including nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and disease-modifying antirheumatic drugs (DMARDs), are commonly prescribed to reduce inflammation and manage pain. NSAIDs, such as ibuprofen and naproxen, help alleviate pain and reduce swelling, making them suitable for both short-term relief and long-term management of symptoms. Corticosteroids, like prednisone, are potent anti-inflammatory agents that can be administered orally or injected directly into the affected joint to provide rapid relief from severe inflammation and pain. However, long-term use of corticosteroids can lead to side effects such as osteoporosis, weight gain, and increased susceptibility to infections, so their use is typically monitored closely by healthcare providers.
In more severe cases, biological response modifiers or biologics may be used to target specific components of the immune system. Biologics, such as tumor necrosis factor (TNF) inhibitors and interleukin (IL) inhibitors, work by blocking the action of specific proteins involved in the inflammatory process, thereby reducing inflammation and preventing joint damage. These medications are often prescribed for individuals with rheumatoid arthritis or other inflammatory types of arthritis who do not respond adequately to traditional DMARDs. Biologics are usually administered via injection or intravenous infusion and require regular monitoring due to potential side effects, including increased risk of infections and possible allergic reactions.
(Physical Therapy and Occupational Therapy)
Alongside medical treatments, physical therapy plays a pivotal role in maintaining joint flexibility and strength. Physical therapists design individualized exercise programs to improve range of motion, strengthen the muscles surrounding the joints, and enhance overall physical function. These exercises can include stretching, strength training, and low-impact aerobic activities such as swimming or cycling. Physical therapy can also incorporate modalities like heat and cold therapy, ultrasound, and electrical stimulation to help reduce pain and improve joint function. Regular physical activity, tailored to the individual’s capabilities and limitations, is crucial in preventing the loss of joint mobility and reducing the risk of disability.
Occupational therapy helps individuals adapt their daily routines to minimize joint strain and maintain independence. Occupational therapists provide practical advice on modifying activities and using assistive devices to make daily tasks easier and less painful. This can include recommending ergonomic tools, splints, or braces to support affected joints and reduce stress during activities. They also teach techniques for joint protection, such as proper body mechanics and energy conservation strategies, to help individuals manage their condition more effectively. By addressing both the physical and functional aspects of arthritis, occupational therapy plays a vital role in improving quality of life and enabling individuals to maintain their independence.
(Advanced Treatments and Surgical Options)
For individuals with severe arthritis who do not respond to conservative treatments, advanced therapies and surgical options may be considered. Hyaluronic acid injections, which act as a lubricant and shock absorber within the joint, can provide relief for some individuals with osteoarthritis, particularly in the knees. Platelet-rich plasma (PRP) therapy and stem cell therapy are emerging treatments that aim to promote healing and regeneration of joint tissues, though more research is needed to establish their long-term efficacy and safety.
In cases where joint damage is extensive and significantly impairs function, surgical interventions may be necessary. Joint replacement surgery, such as total hip or knee arthroplasty, involves removing the damaged joint surfaces and replacing them with artificial components. This procedure can dramatically reduce pain and improve joint function, allowing individuals to regain mobility and enhance their quality of life. Other surgical options include joint fusion, which stabilizes the joint by fusing the bones together, and arthroscopy, a minimally invasive procedure used to diagnose and treat joint problems. Consulting with an orthopedic surgeon can help determine the most appropriate surgical approach based on the individual’s specific condition and needs.
Lifestyle Modifications
Lifestyle changes are equally important in managing arthritis symptoms and improving overall well-being. Regular low-impact exercise, such as swimming, cycling, or walking, can help maintain joint function and reduce stiffness. These activities are gentle on the joints while promoting cardiovascular health, muscle strength, and overall flexibility. Exercise can also help manage pain by stimulating the release of endorphins, the body’s natural painkillers. For individuals with arthritis, it is essential to choose activities that do not exacerbate joint pain and to start slowly, gradually increasing the intensity and duration of exercise as tolerated. In addition to aerobic exercises, incorporating strength training and stretching exercises can further enhance joint stability and mobility.
Weight management is crucial, particularly for those with osteoarthritis, as excess weight exacerbates joint stress. Carrying extra weight increases the load on weight-bearing joints like the knees, hips, and spine, accelerating cartilage wear and tear. Even modest weight loss can significantly reduce joint pain and improve function. A balanced diet rich in anti-inflammatory foods, such as fruits, vegetables, whole grains, and omega-3 fatty acids, can also support joint health and reduce inflammation. Foods high in antioxidants, such as berries and leafy greens, can help combat oxidative stress, which contributes to inflammation. Omega-3 fatty acids, found in fatty fish, flaxseeds, and walnuts, have been shown to reduce joint pain and stiffness in individuals with rheumatoid arthritis. Limiting the intake of processed foods, sugars, and saturated fats is also beneficial, as these can contribute to inflammation and overall poor health.
(Diet and Nutrition)
A balanced diet plays a pivotal role in managing arthritis symptoms and promoting overall health. Anti-inflammatory foods, such as fruits, vegetables, whole grains, and omega-3 fatty acids, can help reduce inflammation and support joint health. Fruits and vegetables are rich in vitamins, minerals, and antioxidants that help combat inflammation and oxidative stress. Leafy greens, berries, and citrus fruits are particularly beneficial. Whole grains, such as quinoa, brown rice, and oats, provide essential nutrients and fiber, helping to maintain a healthy weight and reduce inflammation. Omega-3 fatty acids, found in fatty fish like salmon and mackerel, as well as flaxseeds and chia seeds, have been shown to reduce joint pain and stiffness, especially in individuals with rheumatoid arthritis.
Incorporating a variety of these nutrient-rich foods into the diet can provide the body with the necessary building blocks for repairing and maintaining joint tissues. Conversely, it is important to limit the intake of processed foods, sugars, and saturated fats, as these can increase inflammation and contribute to overall poor health. Processed foods often contain trans fats and refined sugars, which can trigger inflammatory responses in the body. By focusing on a diet rich in whole, unprocessed foods, individuals with arthritis can better manage their symptoms and improve their overall well-being.
(Stress Management and Mental Health)
Managing stress is an integral part of living with arthritis, as chronic pain and limited mobility can significantly impact emotional well-being. Stress management techniques, such as mindfulness, meditation, and yoga, can help mitigate the emotional impact of living with a chronic condition. Mindfulness practices encourage present-moment awareness and can help individuals manage pain and reduce stress. Meditation techniques, such as deep breathing and guided imagery, can promote relaxation and alleviate anxiety. Yoga combines physical movement with breath control and meditation, offering a holistic approach to managing both physical and emotional symptoms of arthritis.
Adequate sleep is also crucial for managing arthritis symptoms and maintaining overall health. Chronic pain can disrupt sleep patterns, leading to fatigue and exacerbating pain and inflammation. Establishing a regular sleep routine, creating a comfortable sleep environment, and practicing good sleep hygiene can help improve sleep quality. Using supportive pillows and mattresses can reduce joint discomfort during the night. Additionally, seeking support from friends, family, and support groups can provide emotional comfort and practical advice for managing arthritis. Connecting with others who understand the challenges of living with arthritis can reduce feelings of isolation and help individuals develop coping strategies.
(Physical Activity and Joint Protection)
Engaging in regular physical activity is essential for maintaining joint health and overall fitness in individuals with arthritis. Low-impact exercises, such as swimming, cycling, and walking, are gentle on the joints while promoting cardiovascular health, muscle strength, and flexibility. These activities can help reduce stiffness, improve range of motion, and manage pain by stimulating the release of endorphins. It is important to choose activities that do not exacerbate joint pain and to start slowly, gradually increasing the intensity and duration of exercise as tolerated. Consulting with a physical therapist can help individuals develop a personalized exercise program that meets their specific needs and limitations.
In addition to aerobic exercises, incorporating strength training and stretching exercises can further enhance joint stability and mobility. Strengthening the muscles around the joints can provide better support and reduce the load on the joints, thereby alleviating pain and preventing further damage. Stretching exercises can help maintain flexibility and prevent stiffness. Using assistive devices, such as braces or splints, can also help protect the joints and reduce strain during daily activities. Occupational therapy can provide practical advice on modifying activities and using ergonomic tools to make daily tasks easier and less painful. By incorporating these lifestyle modifications, individuals with arthritis can enhance their overall well-being and manage their condition more effectively.
Complementary and Alternative Therapies
In addition to conventional medical treatments and lifestyle changes, many individuals with arthritis explore complementary and alternative therapies to alleviate symptoms and improve overall well-being. These therapies often aim to address pain, reduce inflammation, and enhance quality of life through non-traditional methods. Acupuncture, a practice rooted in traditional Chinese medicine, involves inserting thin needles into specific points on the body to stimulate energy flow and promote natural healing. Research suggests that acupuncture may help reduce pain and improve joint function by triggering the release of endorphins and other neurochemicals that modulate pain perception. It is often used as an adjunct therapy to complement conventional treatments, providing relief for those who have not achieved satisfactory results from standard medications alone.
Massage therapy is another popular complementary approach that can provide significant benefits for individuals with arthritis. By applying pressure and manipulating the muscles and soft tissues, massage therapy can enhance circulation, reduce muscle tension, and improve flexibility around affected joints. Techniques such as Swedish massage, deep tissue massage, and myofascial release can help alleviate pain and stiffness, promote relaxation, and support overall physical function. Regular massage sessions can be particularly beneficial for managing the musculoskeletal discomfort associated with arthritis, but it is essential to work with a qualified therapist who understands the specific needs and limitations of arthritis patients.
(Herbal Supplements and Dietary Approaches)
Herbal supplements are widely used by individuals with arthritis seeking natural ways to manage their symptoms. Turmeric, a spice commonly used in curry, contains curcumin, which has been shown to have anti-inflammatory and antioxidant properties. Studies suggest that curcumin can help reduce joint pain and stiffness by inhibiting inflammatory pathways in the body. Similarly, ginger has been used for centuries for its anti-inflammatory effects, and research indicates it may help alleviate arthritis-related pain and inflammation. Both turmeric and ginger can be consumed as part of the diet or taken in supplement form, but it’s crucial to discuss their use with a healthcare provider, as they can interact with other medications and have potential side effects.
Other dietary approaches, such as incorporating omega-3 fatty acids found in fish oil and flaxseed, may also offer relief from arthritis symptoms. Omega-3 fatty acids have been shown to reduce inflammation and improve joint health in individuals with inflammatory arthritis. Additionally, some individuals explore the benefits of a gluten-free or anti-inflammatory diet to manage symptoms, although more research is needed to establish the effectiveness of these dietary changes. Consulting with a nutritionist or dietitian can help tailor a dietary plan to individual needs and ensure that any supplements or dietary adjustments are safe and beneficial.
(Mind-Body Techniques)
Mind-body techniques, including mindfulness, meditation, and yoga, can play a significant role in managing arthritis symptoms and improving overall well-being. Mindfulness and meditation practices focus on enhancing present-moment awareness and reducing stress, which can be particularly beneficial for individuals dealing with chronic pain and emotional strain. Techniques such as deep breathing, progressive muscle relaxation, and guided imagery can help manage pain, reduce anxiety, and promote a sense of calm. Incorporating these practices into a daily routine can enhance coping strategies and improve quality of life.
Yoga, which combines physical postures, breath control, and meditation, offers a holistic approach to managing arthritis. Specific yoga poses can help improve joint flexibility, build strength, and alleviate stiffness. Additionally, yoga can promote relaxation and reduce stress, which can further benefit individuals with arthritis. It is important to work with an experienced yoga instructor who can provide modifications and ensure that the practice is adapted to individual abilities and limitations. Practicing yoga regularly can enhance overall physical and mental well-being, complementing other treatments and lifestyle modifications.
(Safety and Consultation)
While complementary and alternative therapies can offer additional benefits, it is essential to approach them with caution and consult with a healthcare provider before starting any new treatments. Some therapies may interact with conventional medications or have potential side effects, so it is important to ensure that they are safe and appropriate for individual health conditions. A healthcare provider can help evaluate the efficacy of alternative treatments, provide guidance on appropriate use, and monitor for any adverse effects. By integrating complementary therapies with conventional medical care, individuals with arthritis can develop a comprehensive and personalized approach to managing their condition and enhancing their overall quality of life.
Arthritis, with its various forms and underlying causes, presents a significant challenge for those affected, impacting daily life and overall well-being. However, understanding the nuances of arthritis—from its symptoms and causes to the broad spectrum of treatment options—empowers individuals to take proactive steps in managing their condition. Medical treatments, lifestyle modifications, and complementary therapies each play a critical role in alleviating symptoms and improving quality of life.
By integrating these approaches, individuals with arthritis can achieve a more balanced and effective management plan tailored to their unique needs. Regular exercise, weight management, and a healthy diet contribute to overall joint health and function, while complementary therapies offer additional avenues for relief and support. Consulting with healthcare professionals ensures that treatment strategies are both safe and effective, fostering a comprehensive approach to managing arthritis.
Ultimately, a proactive and informed approach to arthritis management can lead to improved physical function, reduced pain, and a better quality of life. Embracing a holistic strategy that combines conventional and alternative treatments with lifestyle changes provides a pathway to living well with arthritis and maintaining a fulfilling and active life despite the challenges of this chronic condition.