Vaccines have revolutionized modern medicine, transforming the landscape of public health by preventing a wide array of infectious diseases. At their core, vaccines function as a sophisticated training system for the immune system, preparing it to recognize and combat specific pathogens without causing the disease itself. This preventive approach has led to remarkable successes, including the eradication of smallpox and significant reductions in the incidence of diseases such as polio and measles.
Despite their profound impact, vaccines are often surrounded by misconceptions and misunderstandings. Some people believe that vaccines can cause the diseases they are meant to prevent or question their necessity in an era of improved sanitation and healthcare. However, the reality is that vaccines play a critical role not only in protecting individuals from severe illness but also in safeguarding entire communities through the concept of herd immunity. By dispelling myths and understanding the science behind vaccines, we can appreciate their importance in maintaining global health and preventing the resurgence of once-controlled diseases.

(wikipedia.org)
How Vaccines Work
Vaccines are pivotal in modern medicine, serving as a cornerstone for preventing infectious diseases. They work by training the immune system to recognize and combat specific pathogens without causing the illness itself. This is accomplished by introducing components of a pathogen—such as proteins, sugars, or genetic material—into the body in a controlled manner. These components are usually weakened, inactivated, or otherwise modified to be harmless. This controlled exposure prompts the immune system to mount a response, creating a defense against future encounters with the actual pathogen. Essentially, vaccines simulate an infection, allowing the body to build immunity without suffering the consequences of the disease.
(Types of Vaccines)
Vaccines come in various forms, each designed to stimulate the immune system in different ways:
-
Inactivated or Killed Vaccines: These vaccines contain pathogens that have been killed or inactivated so that they cannot cause disease. Despite their inactivity, these pathogens still provoke a strong immune response. Examples include the polio vaccine (IPV) and the hepatitis A vaccine.
-
Live Attenuated Vaccines: These vaccines use live pathogens that have been weakened to reduce their ability to cause illness. They closely mimic natural infections, providing a robust immune response. Examples include the MMR vaccine (measles, mumps, rubella) and the oral polio vaccine (OPV).
-
Subunit, Recombinant, or Conjugate Vaccines: These vaccines include only specific parts of the pathogen, such as proteins or sugars, which are enough to stimulate the immune system. They do not contain the whole pathogen. Examples are the human papillomavirus (HPV) vaccine and the Haemophilus influenzae type b (Hib) vaccine.
-
mRNA Vaccines: A more recent innovation, mRNA vaccines use a small segment of genetic material to instruct cells to produce a protein found on the pathogen’s surface. This protein prompts an immune response without using the actual pathogen. Notable examples include the COVID-19 vaccines developed by Pfizer-BioNTech and Moderna.
(Immune Response to Vaccination)
When a vaccine is administered, it triggers the immune system to recognize the introduced components as foreign. The process begins with antigen-presenting cells that process and display these components to other immune cells. Helper T cells are activated in response, which then stimulate B cells to produce antibodies. These antibodies are specific to the antigens introduced by the vaccine and work to neutralize them. Additionally, cytotoxic T cells may be activated to target and destroy cells infected by pathogens. This coordinated immune response helps to eliminate the antigens and prepares the immune system for future encounters.
(Building Immunity Through Memory Cells)
One of the key benefits of vaccination is the creation of memory cells. After the immune system has responded to the vaccine, memory cells are formed and persist long-term. These cells “remember” the pathogen and enable the immune system to respond more quickly and effectively if the individual is exposed to the actual pathogen in the future. This means that the immune system can mount a rapid and potent response, often preventing the disease or mitigating its severity. By effectively “training” the immune system, vaccines provide critical protection against serious illnesses and contribute to broader public health by reducing disease prevalence and transmission within communities. This preparation ensures that the body is equipped to handle real threats with increased efficiency and resilience.
The Role of Vaccines in Preventing Infectious Diseases
(Individual Protection)
Vaccines are instrumental in protecting individuals from the severe effects of infectious diseases, including complications and mortality. For instance, the measles, mumps, and rubella (MMR) vaccine has been a critical tool in significantly reducing the incidence of these diseases. Prior to the widespread use of the MMR vaccine, measles was known for its potential to cause severe complications such as pneumonia, encephalitis, and death. Mumps could lead to complications like orchitis (inflammation of the testicles) and permanent deafness, while rubella posed risks of birth defects when contracted during pregnancy. The introduction of the MMR vaccine has led to dramatic declines in these diseases, showcasing its efficacy in preventing severe outcomes and protecting individual health.
Beyond the MMR vaccine, many other vaccines contribute significantly to individual health. The pneumococcal vaccine, for example, protects against diseases caused by Streptococcus pneumoniae, including pneumonia, meningitis, and bacteremia. For elderly individuals and those with chronic conditions, the influenza vaccine is crucial in reducing the risk of severe flu complications and hospitalization. Vaccines for diseases such as hepatitis B, which can lead to chronic liver infections and cancer, also play a vital role in reducing long-term health impacts. By preventing these diseases, vaccines not only protect individuals but also reduce the overall burden on healthcare systems by decreasing the incidence of serious diseases that require medical treatment.
(Community Protection and Herd Immunity)
On a community level, vaccines play an essential role in establishing herd immunity. Herd immunity occurs when a substantial portion of a population is immunized against a specific pathogen, thus lowering its overall prevalence and reducing the likelihood of an outbreak. When a significant percentage of the population is vaccinated, the spread of the disease is interrupted because there are fewer susceptible individuals for the pathogen to infect. This communal protection is crucial for safeguarding those who cannot be vaccinated due to medical reasons, such as infants who are too young, pregnant women, or individuals with certain medical conditions that contraindicate vaccination.
Herd immunity not only protects individuals who cannot receive vaccines but also helps prevent outbreaks and control the spread of infectious diseases within communities. For example, high vaccination rates have contributed to the control of diseases like polio and measles, which were once common but have become rare in many parts of the world due to effective vaccination programs. The concept of herd immunity underscores the collective responsibility to maintain high vaccination coverage, as each person’s decision to vaccinate contributes to the broader health of the community.
(Impact on Disease Outbreaks)
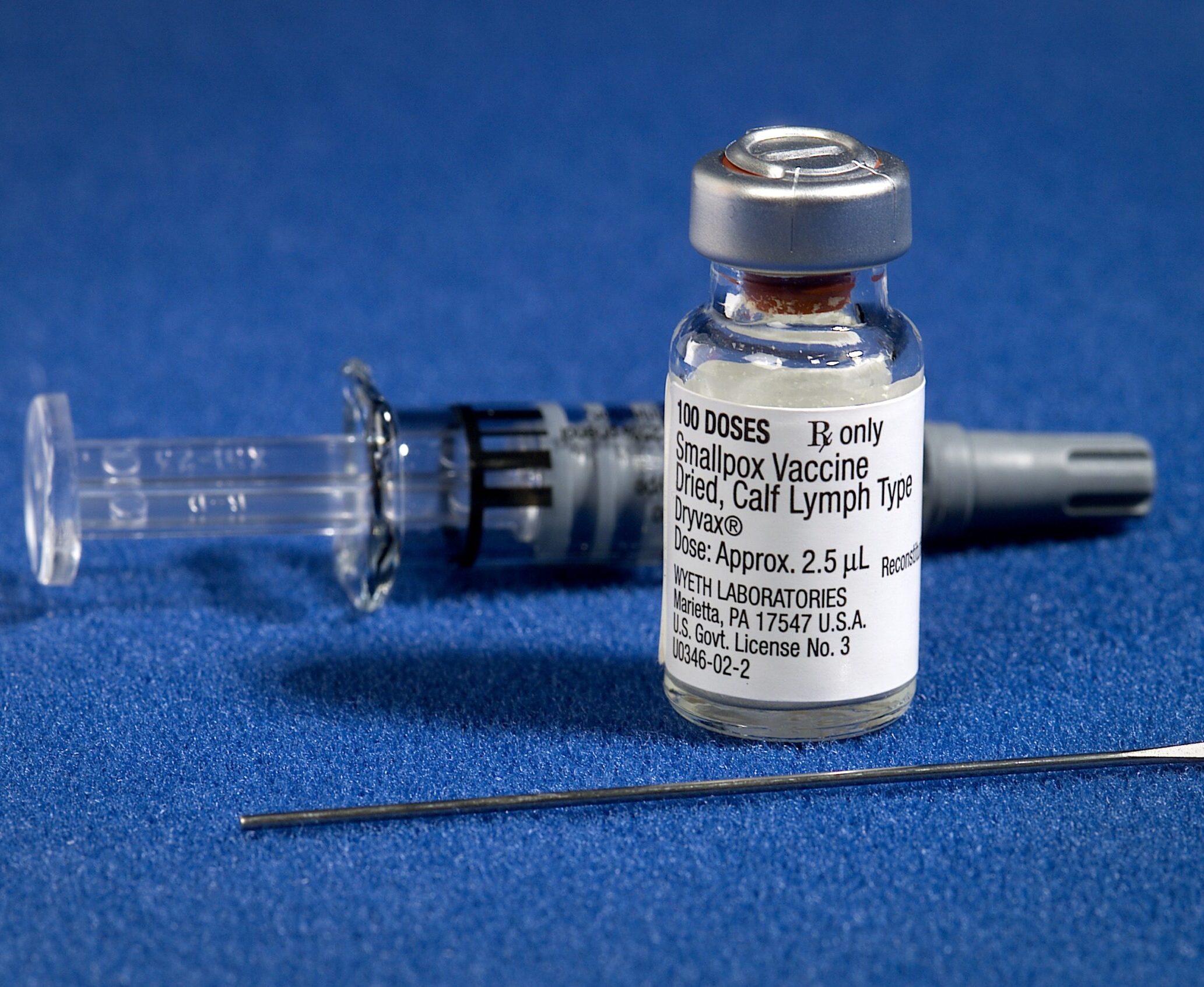
Vaccines have had a profound impact on the management and prevention of disease outbreaks. Historical successes include the eradication of smallpox, a disease that once caused widespread suffering and death. The global smallpox eradication campaign, driven by an aggressive vaccination effort, led to the disease being declared eradicated in 1980. Similarly, the near-eradication of polio highlights the effectiveness of vaccines in controlling diseases that once caused widespread paralysis and death.
Vaccines also play a critical role in responding to emerging and re-emerging infectious diseases. The rapid development and deployment of COVID-19 vaccines were pivotal in controlling the pandemic. Vaccination efforts helped to mitigate severe illness, reduce transmission rates, and prevent healthcare systems from being overwhelmed. The success of vaccines in managing COVID-19 underscores their vital role in controlling pandemics and highlights their importance in public health preparedness.
In summary, vaccines are indispensable tools in the fight against infectious diseases, offering significant benefits at both the individual and community levels. They protect individuals from severe health outcomes and complications while contributing to herd immunity, which shields vulnerable populations and helps prevent outbreaks. The ongoing success of vaccination programs in controlling and eliminating diseases emphasizes the crucial role vaccines play in maintaining public health and ensuring a safer future for communities around the world.
The Importance of Immunization for Public Health
(Foundations of Public Health)
Immunization stands as a cornerstone of public health, forming the basis for many successful disease prevention strategies. Its impact is evident through widespread vaccination programs that have transformed the landscape of global health. For instance, the eradication of smallpox in 1980 represents one of the most significant achievements in public health history. This was made possible by a concerted global vaccination effort, demonstrating how coordinated immunization campaigns can lead to the complete elimination of a disease. Smallpox was a devastating illness that once caused millions of deaths and severe disfigurement. Its eradication is a testament to the power of vaccines and their role in controlling and eliminating infectious diseases.
In addition to smallpox, vaccination efforts have led to significant reductions in other serious diseases. For example, polio, a virus that can cause paralysis and death, has been reduced by over 99% worldwide thanks to an extensive vaccination campaign. The global initiative to eradicate polio has brought the world closer to eliminating this crippling disease. Similarly, the incidence of whooping cough (pertussis) has decreased markedly in many countries due to effective vaccination programs. These successes illustrate the profound impact that immunization has on reducing the prevalence of dangerous diseases and improving public health outcomes.
(Reducing Healthcare Burden)
Vaccines not only protect individuals but also alleviate the strain on healthcare systems by preventing disease outbreaks and the associated costs of medical treatments. Preventing diseases through vaccination reduces the need for medical interventions, hospitalizations, and long-term care, thus lowering healthcare expenses. For instance, childhood vaccines have substantially decreased the incidence of diseases that previously required expensive and resource-intensive treatments. By preventing outbreaks, vaccines reduce the need for emergency responses and large-scale medical efforts, allowing healthcare resources to be allocated more effectively.
Moreover, vaccines contribute to the overall efficiency and sustainability of healthcare systems. By controlling diseases that would otherwise lead to significant illness and disability, vaccines help maintain a healthier population and reduce the economic burden associated with treating preventable diseases. This is particularly important in regions with limited healthcare resources, where the cost of managing outbreaks can be overwhelming. Vaccination programs thus play a crucial role in ensuring that healthcare systems can manage resources efficiently and provide care for a broader range of health needs.
(Protecting Vulnerable Populations)
Immunization is particularly critical for protecting vulnerable populations, including infants, the elderly, and individuals with compromised immune systems. For these groups, even mild diseases can lead to severe complications or death. Vaccines offer a vital layer of protection against diseases that can be especially dangerous for these individuals. For example, the pneumococcal vaccine protects against pneumonia and meningitis, which are particularly severe for the elderly and those with chronic health conditions. Similarly, vaccines for diseases like influenza and whooping cough are crucial for safeguarding young children and older adults, who are at higher risk of severe outcomes.
In regions with limited healthcare resources, vaccines play an essential role in preventing disease spread and improving overall health. Access to vaccines in these areas can prevent outbreaks that might otherwise overwhelm local healthcare systems. By reducing the incidence of infectious diseases, vaccines help ensure that vulnerable populations are less likely to suffer from preventable illnesses and complications.
(Global Health and Future Prospects)
The role of immunization extends beyond individual and community health; it is a key component of global health strategies. As new vaccines are developed and introduced, the potential for further advancements in disease prevention grows. Continued investment in vaccine research, development, and distribution is essential for addressing emerging health threats and improving global health outcomes. Vaccines have the power to prevent pandemics, control disease outbreaks, and ultimately contribute to a healthier, more resilient world.
In summary, immunization is a fundamental element of public health that has led to the eradication of diseases, significant reductions in others, and a reduced burden on healthcare systems. Its impact is profound, offering protection to individuals and communities, alleviating healthcare costs, and safeguarding vulnerable populations. The ongoing success of vaccination programs underscores their importance in advancing public health and highlights the need for continued support and innovation in immunization efforts worldwide.
Addressing Common Misconceptions
(Myth: Vaccines Cause the Diseases They Are Meant to Prevent)
One prevalent misconception is that vaccines can cause the very diseases they are designed to protect against. This myth often stems from confusion about how vaccines work. In reality, vaccines contain either inactivated (killed) or weakened (live attenuated) components of pathogens, such as proteins or genetic material. These components are specifically modified to stimulate an immune response without causing the actual disease.
For instance, inactivated vaccines, such as the polio vaccine (IPV) and the hepatitis A vaccine, use pathogens that have been completely destroyed so they cannot cause illness. Live attenuated vaccines, like the MMR (measles, mumps, rubella) vaccine, contain live pathogens that have been weakened to the point where they cannot cause disease in healthy individuals. The mild symptoms that sometimes follow vaccination, such as a low-grade fever or a sore arm, are generally signs of the immune system engaging with the vaccine and building immunity, not symptoms of the disease itself. These reactions are usually brief and much less severe than the diseases they protect against.
(Myth: Vaccines Are Unnecessary Due to Improved Sanitation and Healthcare)
Another common misconception is that advancements in sanitation and healthcare have made vaccines unnecessary. While improvements in sanitation, hygiene, and healthcare are vital for overall health, they do not eliminate the risk of infectious diseases entirely. For example, despite the availability of clean water and improved living conditions, diseases like measles and whooping cough can still spread rapidly if vaccination rates drop.
Vaccines provide an essential layer of protection that complements these public health measures. They are crucial for maintaining control over diseases that could otherwise resurge. The decline in vaccination coverage can lead to outbreaks of diseases that were once under control. For instance, recent years have seen a resurgence of measles in certain areas due to reduced vaccination rates. This highlights the importance of vaccines in disease prevention, even in the context of overall improvements in public health.
(Myth: Natural Immunity is Better Than Vaccine-Induced Immunity)
Some individuals believe that natural immunity, which occurs after contracting and recovering from a disease, is superior to vaccine-induced immunity. While natural immunity can provide protection, it often comes at the cost of experiencing the disease’s symptoms and potential complications. Diseases such as chickenpox and pertussis (whooping cough) can lead to serious health issues, including hospitalization or long-term effects. Vaccines offer a way to develop immunity without undergoing the full disease experience, minimizing the risk of severe health outcomes.
Furthermore, vaccines are specifically designed to provide targeted and safe immunity. They stimulate a robust immune response without causing the disease, often resulting in long-lasting protection. In contrast, natural infection can result in more severe outcomes and is not always a reliable way to achieve immunity.
(Myth: Vaccines Contain Harmful Ingredients)
Concerns about vaccine ingredients are another common source of misinformation. Some people worry that vaccines contain harmful substances, such as mercury or aluminum. While vaccines do contain small amounts of additives and preservatives, these are present in quantities deemed safe by regulatory agencies. For instance, thimerosal, a mercury-containing compound, was used as a preservative in some vaccines but has been removed or reduced to trace amounts in most vaccines due to public concern, even though research has shown it to be safe. Aluminum compounds are used as adjuvants to enhance the immune response and have been thoroughly tested for safety. The amounts used in vaccines are well below levels that could cause harm.
Regulatory agencies like the U.S. Food and Drug Administration (FDA) and the World Health Organization (WHO) rigorously evaluate vaccine ingredients to ensure their safety and efficacy. These evaluations involve extensive research and clinical trials to confirm that vaccines are both effective in preventing disease and safe for public use.
(Myth: Vaccines Are Only Necessary for Children)
Some people believe that vaccines are only important during childhood. However, vaccination is important throughout life. Booster doses are often required to maintain immunity against certain diseases, and some vaccines are recommended for adults, such as the influenza vaccine and vaccines for diseases like shingles or pneumococcal infections. For instance, the tetanus-diphtheria-pertussis (Tdap) booster is recommended every ten years for adults to maintain protection. Vaccination strategies are designed to ensure ongoing protection as individuals age and their immunity may wane.
In summary, addressing misconceptions about vaccines is crucial for maintaining public health. Understanding how vaccines work, their role in disease prevention, and the safety of their ingredients can help dispel myths and promote informed decision-making. Vaccines are a powerful tool in protecting individual and community health, and overcoming misinformation is essential for continuing their success in preventing infectious diseases.
Conclusion
In summary, vaccines are a cornerstone of public health, offering a powerful means of preventing infectious diseases and improving overall well-being. Their role in reducing the incidence of severe illnesses, controlling disease outbreaks, and contributing to herd immunity underscores their significance in modern medicine. The successes of vaccination programs, from the eradication of smallpox to the near-elimination of polio, highlight their transformative impact on global health.
Addressing common misconceptions and understanding the science behind vaccines are crucial for maintaining public trust and ensuring continued progress in disease prevention. By recognizing the benefits of vaccines and overcoming misinformation, we can safeguard both individual and community health, ensuring that the achievements of vaccination efforts are sustained for future generations. Vaccines not only protect us from immediate health threats but also contribute to a healthier, more resilient world, reflecting the enduring importance of immunization in advancing public health.