Throughout history, humanity has faced numerous health crises caused by deadly diseases that have shaped the course of events and left profound impacts on societies. From ancient pandemics to modern health emergencies, these diseases have tested medical science and public health systems, revealing both the vulnerabilities and resilience of populations worldwide. In this exploration of the ten deadliest diseases, we delve into the pathogens responsible, their modes of transmission, and the toll they have taken on human lives.
The impact of these diseases extends beyond mere statistics; they have influenced historical events, driven scientific discoveries, and reshaped global health policies. Understanding these diseases—ranging from the historical plague pandemics to contemporary threats like HIV/AIDS and COVID-19—provides crucial insights into how they have challenged humanity and highlights the ongoing efforts to combat and prevent such threats.
This article provides a detailed examination of each disease, outlining their mortality rates, transmission methods, and historical significance. By exploring the deadliest diseases, we gain a greater appreciation for the advancements in medicine and public health that have emerged in response to these global challenges. From the eradication of smallpox to the ongoing battle against malaria, the story of these diseases is also a testament to human ingenuity and perseverance in the face of adversity.
1. Smallpox

(wikipedia.org)
Smallpox, caused by the Variola virus, stands as one of the most deadly diseases in human history. The virus is highly contagious and was responsible for devastating epidemics across continents. Smallpox is characterized by a high fever and a distinctive rash that progresses to pus-filled lesions. Historically, the mortality rate of smallpox was alarmingly high, with estimates indicating that 30% or more of those infected succumbed to the disease. Its impact was profound, leading to significant loss of life and widespread fear.
The history of smallpox is marked by its devastating effects on populations. The disease ravaged societies from ancient times through the 20th century. Epidemics swept through communities, causing severe illness and death. Smallpox not only affected individual health but also had far-reaching social and economic consequences. The disease’s high mortality rate and ability to spread rapidly made it a persistent threat to public health.
The turning point in the battle against smallpox came with the development and implementation of a global vaccination program. Edward Jenner’s pioneering work in the late 18th century, which demonstrated the effectiveness of using cowpox to confer immunity, laid the groundwork for the development of smallpox vaccines. By the mid-20th century, a coordinated global effort led by the World Health Organization (WHO) succeeded in eradicating the disease. The last known natural outbreak occurred in Somalia in 1977, and smallpox was officially declared eradicated in 1980.
The eradication of smallpox represents a monumental achievement in the field of medicine and public health. It serves as a testament to the power of vaccination and global cooperation in combating infectious diseases. Smallpox remains the only human disease to have been eradicated entirely, highlighting the potential for similar success against other deadly pathogens with continued dedication and effort.
2. Plague

(commons.wikipedia)
The plague, caused by the bacterium Yersinia pestis, is a highly lethal disease known for its devastating impact on human populations throughout history. This pathogen has caused several significant pandemics, with varying strains leading to different forms of the disease. The three main types of plague—bubonic, septicemic, and pneumonic—each present severe health risks, with mortality rates that can reach up to 90% in the case of untreated septicemic plague. The disease is primarily transmitted through flea bites, but can also spread through contact with infected animals or humans.
One of the most notorious outbreaks of plague in history was the Black Death, which swept through Europe between 1347 and 1351. This pandemic is estimated to have killed between 25 and 30 million people, representing a substantial portion of Europe’s population at the time. The Black Death’s rapid spread and high mortality rate had profound social, economic, and cultural effects. Entire communities were decimated, and the epidemic led to significant shifts in labor markets and social structures, with long-lasting repercussions on European society.
The plague’s impact extended beyond Europe, affecting regions across Asia and Africa. The disease is thought to have originated in the steppes of Central Asia, spreading along trade routes such as the Silk Road. As it traveled, it inflicted heavy casualties on populations, contributing to widespread fear and societal disruption. The plague’s ability to cause widespread death and suffering made it a prominent factor in shaping historical events and societal changes.
In modern times, while the plague is no longer a global threat thanks to advancements in medicine and hygiene, it still occurs sporadically in some regions. Continued surveillance, prompt treatment with antibiotics, and public health measures are essential to managing and controlling outbreaks. The legacy of the plague underscores the importance of addressing infectious diseases and preparing for potential re-emergences of historic pathogens.
3. Spanish Flu (1918 Influenza Pandemic)

(rawpixel.com)
The Spanish Flu, caused by the H1N1 influenza virus, remains one of the most catastrophic pandemics in modern history. Occurring in 1918, this influenza pandemic spread rapidly across the globe, infecting about one-third of the world’s population. The virus was highly virulent, leading to an estimated 50 million deaths worldwide. Its impact was exacerbated by the conditions of World War I, which facilitated the spread of the virus through crowded military camps and trenches.
The Spanish Flu was unusual not only for its high transmission rate but also for its pattern of mortality. Unlike typical influenza strains, which predominantly affect the very young and the elderly, the Spanish Flu had a high mortality rate among healthy young adults. This led to a significant loss of life in a demographic typically less vulnerable to such infections. The pandemic’s severity was compounded by the limited medical knowledge and resources available at the time, including the lack of effective vaccines and antiviral treatments.
The pandemic’s effects were profound, causing widespread social and economic disruptions. Public health responses varied, with some areas implementing quarantine measures, mask mandates, and restrictions on public gatherings. The pandemic also highlighted the need for improved public health infrastructure and response strategies, setting the stage for future advancements in disease control and prevention. The Spanish Flu’s global reach and devastating impact prompted significant research into influenza and pandemic preparedness.
In the aftermath of the Spanish Flu, the world saw considerable improvements in medical science and public health. Vaccines and antiviral medications developed in subsequent decades have helped to mitigate the impact of future influenza outbreaks. The 1918 pandemic serves as a stark reminder of the potential for global health crises and underscores the importance of vigilance, research, and preparedness in managing infectious diseases.
4. HIV/AIDS
(flickr.com)
HIV/AIDS, caused by the Human Immunodeficiency Virus (HIV), has had a profound impact on global health since its emergence in the early 1980s. HIV attacks the immune system, specifically targeting CD4 cells, which are crucial for immune function. As the virus progresses, it leads to Acquired Immunodeficiency Syndrome (AIDS), a stage where the immune system is severely compromised, making individuals highly susceptible to opportunistic infections and certain cancers. Without effective treatment, HIV progresses to AIDS with a high mortality rate, as patients often face life-threatening complications.
The global impact of HIV/AIDS has been significant, with over 36 million deaths attributed to the epidemic since its identification. The disease has particularly affected sub-Saharan Africa, which remains the region most burdened by HIV/AIDS. Efforts to combat the epidemic have focused on increasing access to antiretroviral therapy (ART), which has transformed HIV from a fatal disease into a manageable chronic condition for many. ART helps to suppress viral loads, restore immune function, and significantly improve the quality of life for those living with HIV.
Despite advances in treatment, the HIV/AIDS epidemic continues to pose major challenges. Stigma, discrimination, and inadequate access to healthcare in some regions hinder prevention and treatment efforts. Global initiatives have worked to address these issues by promoting education, providing free or low-cost treatment, and supporting vulnerable populations. Prevention strategies, including the use of condoms, harm reduction for people who inject drugs, and pre-exposure prophylaxis (PrEP), are crucial in reducing new infections and controlling the spread of the virus.
The ongoing fight against HIV/AIDS highlights the need for continued research, funding, and global cooperation. While significant progress has been made, challenges remain in ensuring equitable access to treatment and prevention measures. Addressing these issues and continuing to advance scientific research are essential steps in working towards an end to the HIV/AIDS epidemic and improving the lives of those affected by this devastating disease.
5. Ebola Virus Disease (EVD)

(pxhere.com)
Ebola Virus Disease (EVD), caused by the Ebola virus, is a severe and often fatal illness characterized by its high mortality rate. The disease manifests with sudden onset of fever, severe weakness, and muscle pain, followed by vomiting, diarrhea, and, in severe cases, bleeding and organ failure. The Ebola virus is transmitted through direct contact with the blood, body fluids, or tissues of infected animals or humans, making its spread particularly challenging in areas with limited healthcare infrastructure.
The Ebola virus has several strains, each varying in virulence and fatality. The mortality rate for Ebola can range from 25% to 90%, depending on the outbreak and the specific strain involved. One of the most notable outbreaks occurred between 2014 and 2016 in West Africa. This outbreak, primarily affecting Guinea, Liberia, and Sierra Leone, resulted in over 11,000 deaths and overwhelmed local health systems. The crisis prompted a massive international response, including medical aid, public health campaigns, and the development of experimental treatments and vaccines.
The impact of the Ebola outbreak extended beyond the immediate health crisis, affecting economies, social structures, and healthcare systems in the affected regions. The epidemic highlighted the need for improved disease surveillance, rapid response capabilities, and stronger healthcare infrastructure to manage such outbreaks. The global response included the deployment of medical personnel, establishment of treatment centers, and implementation of strict infection control measures to curb the spread of the virus.
Advancements in the fight against Ebola include the development and deployment of vaccines, such as the rVSV-ZEBOV vaccine, which has shown efficacy in protecting against the virus. Continued research and preparedness are crucial to managing future outbreaks and minimizing the impact of Ebola. Efforts to strengthen healthcare systems and improve global collaboration are essential in ensuring a swift and effective response to potential Ebola outbreaks, safeguarding both affected populations and the global community.
6. Tuberculosis (TB)

(commons.wikipedia)
Tuberculosis (TB), caused by the bacterium Mycobacterium tuberculosis, remains one of the most persistent and deadly infectious diseases globally. TB primarily affects the lungs, but it can also impact other parts of the body, including the kidneys, spine, and brain. The disease is transmitted through airborne droplets when an infected person coughs or sneezes, making it highly contagious, especially in crowded or poorly ventilated environments. If left untreated, TB can be fatal, with a mortality rate of approximately 15-20% in untreated cases.
Despite the availability of effective treatments, TB continues to be a major health issue, causing about 1.5 million deaths annually. The persistence of the disease is partly due to challenges in diagnosis, treatment adherence, and the emergence of drug-resistant strains. Multidrug-resistant TB (MDR-TB) and extensively drug-resistant TB (XDR-TB) complicate treatment, as these strains do not respond to the standard antibiotics used to treat TB, necessitating longer and more complex treatment regimens.
Efforts to control TB have included widespread use of antibiotics and the development of new treatments. Directly Observed Therapy Short-course (DOTS) has been a cornerstone of TB control programs, ensuring patients adhere to their treatment regimens. The BCG vaccine, while not universally effective, provides some protection against severe forms of TB, especially in children. Public health initiatives also focus on improving diagnostic methods, such as molecular tests that can quickly identify drug-resistant strains, and strengthening healthcare systems to support TB patients.
The fight against TB highlights the need for continued investment in research, healthcare infrastructure, and public health policies. Addressing TB requires a multifaceted approach, including better diagnostics, effective treatments, and comprehensive public health strategies to reduce transmission and improve patient outcomes. By enhancing global efforts and resources dedicated to TB control, it is possible to reduce the burden of this disease and save lives around the world.
7. Malaria
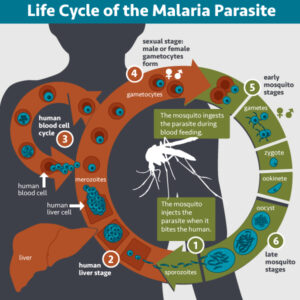
(flickr.com)
Malaria is a life-threatening disease caused by Plasmodium parasites, transmitted to humans through the bites of infected Anopheles mosquitoes. The disease presents with a range of symptoms, including high fever, chills, and flu-like illness, which can escalate to severe complications such as organ failure and cerebral malaria. Malaria is endemic in tropical and subtropical regions, particularly in sub-Saharan Africa, where the majority of cases and deaths occur. The mortality rate varies, with severe cases having a death rate as high as 10% if untreated, underscoring the disease’s potential severity.
Malaria remains a major global health challenge, with over 200 million cases reported annually and approximately 400,000 deaths each year. The high burden of the disease is attributed to factors such as inadequate access to healthcare, poor mosquito control measures, and resistance to antimalarial drugs and insecticides. Plasmodium falciparum, one of the four species of Plasmodium parasites that cause malaria in humans, is particularly dangerous due to its ability to cause severe and often fatal disease.
Efforts to combat malaria have focused on both prevention and treatment. Preventive measures include the use of insecticide-treated bed nets, indoor spraying with insecticides, and environmental management to reduce mosquito breeding sites. Treatment typically involves antimalarial drugs such as artemisinin-based combination therapies (ACTs), which are effective against the parasite. However, the emergence of drug-resistant strains poses a significant challenge, necessitating ongoing research into new treatments and strategies.
The global fight against malaria requires a coordinated approach involving public health initiatives, research, and community engagement. Enhanced surveillance, rapid diagnostic tests, and the development of vaccines are crucial components in reducing the incidence and mortality of malaria. Continued investment in these areas, along with strengthening healthcare systems and addressing social determinants of health, is essential for achieving long-term control and eventual eradication of the disease.
8. Rabies
(commons.wikipedia)
Rabies is a severe viral disease caused by the rabies virus, which belongs to the Lyssavirus genus. The disease is transmitted primarily through the bite or scratch of an infected animal, commonly dogs, bats, or other mammals. Once the virus enters the body, it travels along peripheral nerves to the central nervous system, leading to a range of symptoms including fever, headache, and anxiety, followed by more severe neurological symptoms such as confusion, hallucinations, paralysis, and hydrophobia. The progression of the disease is rapid and often fatal, with a mortality rate approaching 100% once clinical symptoms have appeared.
Rabies is a preventable disease, and its fatality underscores the importance of prompt intervention. Immediate and thorough washing of the wound with soap and water is the first critical step in preventing the virus from advancing. Following this, post-exposure prophylaxis (PEP) with a series of rabies vaccines and, if necessary, rabies immune globulin is highly effective in preventing the onset of symptoms and ensuring survival. PEP must be administered promptly after exposure to be effective, highlighting the importance of seeking medical attention without delay.
Globally, rabies remains a significant public health issue, particularly in regions with limited access to healthcare and vaccination. While rabies has been largely controlled in many developed countries through widespread vaccination of pets and wildlife control programs, it continues to pose a threat in parts of Asia and Africa. In these areas, efforts are focused on increasing access to vaccines, improving animal control programs, and enhancing public awareness to reduce the incidence of the disease.
The global response to rabies includes initiatives by organizations such as the World Health Organization (WHO) and various non-governmental organizations. Strategies involve mass vaccination of domestic animals, community education, and the development of better diagnostic tools and vaccines. Continued investment in these areas, along with international collaboration, is essential to combat rabies and reduce its impact on global health.
9. COVID-19

(pxhere.com)
COVID-19, caused by the SARS-CoV-2 virus, has emerged as one of the most significant global health crises of the 21st century. The disease, first identified in Wuhan, China in late 2019, rapidly spread across the globe, leading to widespread illness, disruption, and loss of life. COVID-19 primarily transmits through respiratory droplets when an infected person coughs, sneezes, or talks, and it can also spread through contact with contaminated surfaces. Symptoms range from mild respiratory issues to severe pneumonia, and the disease can lead to long-term complications or death, particularly in vulnerable populations.
The mortality rate for COVID-19 is approximately 1-3%, but this figure varies significantly by region, age group, and underlying health conditions. Older adults and individuals with pre-existing health conditions, such as cardiovascular disease or diabetes, face higher risks of severe outcomes and death. The pandemic has placed immense pressure on healthcare systems worldwide, leading to shortages of medical supplies, overwhelmed hospitals, and increased strain on healthcare workers. The varied impact of the virus has also highlighted disparities in healthcare access and resources across different regions.
The global response to COVID-19 has involved unprecedented efforts in public health, research, and international collaboration. Vaccines developed at remarkable speed have played a crucial role in controlling the spread of the virus and reducing severe illness and death. Vaccination campaigns, along with public health measures such as social distancing, mask-wearing, and travel restrictions, have been central to managing the pandemic. However, the emergence of new variants has posed additional challenges, emphasizing the need for ongoing surveillance, booster doses, and updated vaccines.
As the world continues to navigate the effects of COVID-19, efforts are focused on achieving widespread vaccination, enhancing treatments, and preparing for future pandemics. The lessons learned from this global health crisis will inform strategies for managing infectious diseases and strengthening global health systems. The pandemic underscores the importance of preparedness, research, and international cooperation in addressing public health challenges and protecting global well-being.
10. Cholera

(flickr.com)
Cholera, caused by the bacterium Vibrio cholerae, is an acute diarrheal disease known for its rapid onset and severe symptoms. The primary mode of transmission is through ingestion of contaminated water or food, typically in regions with inadequate sanitation and clean water supplies. Once inside the body, the bacteria release toxins that cause severe, watery diarrhea and vomiting. This leads to rapid dehydration and electrolyte imbalance, which can be life-threatening if not promptly addressed.
Without treatment, cholera can have a high mortality rate, potentially reaching up to 50% due to the rapid progression of dehydration and shock. However, with timely and appropriate treatment, the mortality rate drops to less than 1%. The cornerstone of treatment is rehydration therapy, which involves administering oral rehydration salts (ORS) or intravenous fluids to replace lost fluids and electrolytes. In severe cases, antibiotics may also be used to shorten the duration of symptoms and reduce the severity of the illness.
Cholera outbreaks often occur in regions affected by poor sanitation and limited access to clean water. The disease is particularly prevalent in areas where water sources are contaminated with fecal matter. Efforts to control cholera focus on improving water, sanitation, and hygiene (WASH) infrastructure, as well as promoting good hygiene practices and ensuring access to safe drinking water. Public health campaigns and educational initiatives play a crucial role in preventing outbreaks and managing cholera cases effectively.
The development and distribution of cholera vaccines also contribute to controlling the disease, particularly in high-risk areas. Vaccination, combined with improvements in sanitation and health education, helps reduce the incidence of cholera and mitigate its impact. Continued investment in these areas, along with global cooperation to address water and sanitation challenges, is essential in combating cholera and protecting public health, especially in vulnerable communities.
Conclusion,
The history of humanity is intricately linked with the struggle against deadly diseases that have shaped societies, influenced historical events, and driven advancements in medical science. From the devastating impacts of diseases like the Black Death and smallpox to the ongoing challenges posed by modern threats such as HIV/AIDS and COVID-19, these illnesses have tested the limits of public health systems and highlighted the critical need for vigilance, innovation, and global cooperation.
Understanding these ten deadliest diseases not only sheds light on their historical and contemporary significance but also underscores the progress made in combating them. Advances in medical research, treatment, and preventive measures have transformed how we approach and manage these health crises, turning once-fatal conditions into manageable chronic illnesses and, in some cases, eradicating them entirely. The global response to these diseases reveals the resilience and adaptability of humanity, as well as the importance of continued investment in healthcare infrastructure, education, and international collaboration.
As we continue to face emerging health threats and navigate the challenges of ongoing epidemics, the lessons learned from past and present diseases will guide our efforts in improving global health. By remaining informed and proactive, we can build on past successes and work towards a future where the impact of such deadly diseases is significantly reduced, ensuring better health outcomes for communities worldwide.


